"Anyone willing to be corrected is on the pathway to life. Anyone refusing has lost his chance."
-Proverbs 10:17
"We are training a group of physicians who have never been observed"
-Ludwig Eichna, MD
Today marks the first of a series of posts on feedback. I had initially planned on a single post but as I dug deep into the literature, I realized that there is far too much good stuff for a single post.
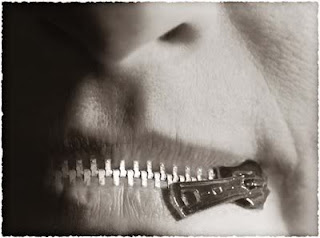
Feedback is such a hot topic in the medical education literature. We pay a lot of attention to it, yet students still rate our feedback skills as mediocre at best. They want feedback, and from what I've seen clinically, they NEED feedback. Unfortunately, as in many educational endeavors, we haven't been trained in appropriate techniques. Even with training, learners will often miss the fact that they've even received feedback.
Feedback is an essential component to improvement. Without insight into our failures and successes we fall into a routine and make the same errors over and over.
So what is feedback and why does it matter?
August 12, 1983: A Call to Arms. It was on this day in JAMA that Jack Ende, MD, published what is possibly the most referenced article on feedback. His work is still relevant today.
He defines feedback as "An informed, nonevaluative, and objective appraisal of performance that is aimed at improving clinical skills rather than estimating the students personal worth."
The above definition highlights some keys to good feedback:
Informed and objective: Feedback is based upon first person observations of skills, behaviors, and attitudes. Without this first person account, a student will tend to discount the value of the feedback.
Nonevaluative: Feedback is much different from evaluation. Evaluation is a summative judgment that occurs at the completion of a period of time. Feedback is formative; it allows the learner to identify areas in need of improvement in real time without fear of a negative evaluation.
Aimed at improving clinical skills: The skills we need to master to become a competent physician are so vast that it is almost overwhelming. Feedback helps to accelerate the process by offering tips and pearls for improvement.
Dr. Ende also includes his guidelines for giving feedback within the article.
Feedback Should:
1. Be undertaken with the teacher and the learner working as allies, with common goals
Start each shift by finding out what skills your learner wants to focus on. This gives the learner an active role and allows you to create a metric for feedback later in the shift.
2. Be well timed and expected
Feedback should be expected by the learner, or better, solicited by the learner. An understanding on the teacher part is needed to avoid times when the learner is not overly stressed.
3. Based on first hand data
The best person to provide feedback is the person who observed the trainees performance. This is often the same person experienced enough to make relevant observations of performance.
4. Regulated in quantity and limited to behaviors that are remediable
Keeping feedback short and limited to only 1-3 behaviors or skills needing improvement allows for the learner to make the needed corrections without overwhelming them with information.
5. Phrased in descriptive, nonevaluative language
Care should be taken to word the feedback effectively in a nonjudgemental fashion. "Your differential did not include _____" is much better than "Your differential is limited and needs a lot of work."
6. Deal with specific performances, not generalizations
How often do you hear "Good job today" as the only feedback a student gets? While good for the individual ego, this kind of feedback is useless when if comes to effecting improvement. Focus on "actions" in order to provide more effective feedback. Statements that allow for psychological distance are helpful as well. For example,"The choice of sux for a paralytic in this dialysis patient didn't account for the possibility that he may have hyperkalemia" is better than "You completely failed to consider the contraindications to sux when performing RSI on this patient."
7. Offer subjective data, labeled as such
When offering subjective data, make sure to use "I" statements, especially when offering personal opinions or reactions. Consider the following: "While watching you perform the history, I felt that you were uncomfortable addressing the sexual history" vs "You looked uncomfortable addressing the sexual history." The latter statement could give the learner the fear that their discomfort was on show for all to see.
8. Deal with decisions and action, rather than assumed intentions or interpretations
By focusing on the decisions or actions, and not the learner per se, the learner and teach can review the effects of the decision without assigning blame and inducing psychological protection mechanisms that would prevent to learner from accepting the feedback.
Feedback is an essential part of learner improvement. While Dr. Eichna identified the problem with the lack of observation more than 30 years ago, he missed the fact that even when observed, faculty fail to offer insights for improvement. This is where the value of good feedback skills becomes mandatory. Without it, mistakes continue uncorrected, sound practice is not reinforced, and the students rarely become clinically competent. Feedback is hard, but not as hard as some believe. With practice, these skills will become second nature and you will make a difference in the care of thousands of patients.
Reference:
Reference:
Ende J. Feedback in clinical medical education. JAMA. 1983 Aug 12;250(6):777-81. PMID: 6876333 [PubMed - indexed for MEDLINE]